All articles
How Health Benefits Strategy Shifts As Employers Focus On Simplicity And Better Coordination
Erika Poole, Founder and CEO of Spectacle Health, explains how ICHRA and smarter benefits design give employees more choice and help employers manage rising healthcare costs.
Key Points
Rising healthcare costs and complex benefits mean employees underutilizing coverage, creating hidden inefficiencies for employers.
Erika Poole, Founder and CEO of Spectacle Health, emphasizes that flexible strategies such as phased ICHRA adoption and thoughtful plan pairing help control costs while expanding choice.
Poole argues that employers improve outcomes by educating teams on how to use benefits, simplifying plan designs, leveraging supplemental coverage, and offering guidance through healthcare navigators.
There’s a real opportunity in better coordination. People freak out about deductibles, but they don’t realize you can pair plans with things such as accident or indemnity coverage to take the bite out of a major event.
The pressure on employer health plans is no longer just about rising costs. Employees consistently say they want more support from their benefits, yet many struggle to understand or use what’s already available. The problem is not a lack of offerings, but fragmented design and unclear communication that turn well-intentioned benefits into a source of confusion instead of value.
Erika Poole, Founder and CEO of Spectacle Health, helps employers rethink health benefits through more flexible, employee-centered approaches. Before founding Spectacle Health, Poole led UX research and innovation at Elevance Health across both group and individual-market products, and previously served as an Assistant Professor at Penn State University specializing in health informatics. Poole points out that healthcare costs are driven largely by pharmacy spend, cancer care, and chronic disease management.
"There’s a real opportunity in better coordination. People freak out about deductibles, but they don’t realize you can pair plans with things such as accident or indemnity coverage to take the bite out of a major event," says Poole. She says alternatives to traditional fully insured models can help rebalance both cost and coverage. "You could pair a direct primary care subscription with more catastrophic coverage for services that fall outside of what DPC covers," she explains.
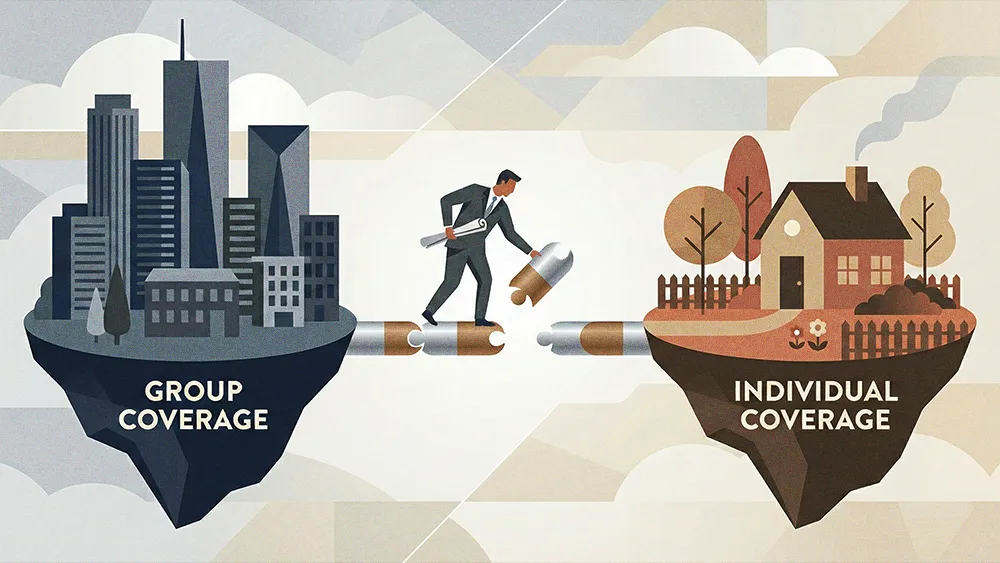
Solutions such as ICHRA are gaining traction as employers rethink not just what benefits they offer but how those benefits are delivered. Rather than enrolling everyone in the same group plan, ICHRA gives employees more choice and control. Poole points to this flexibility as a better fit for today’s workforce, especially as teams become more distributed and employee needs become more varied.
Phased adoption: Poole explains that ICHRA doesn’t have to be rolled out all at once. Employers can introduce it gradually, preserving stability for current employees while offering ICHRA to new hires or specific groups. "One thing employers should keep in mind with ICHRA is that it’s not an all-or-nothing thing,” she advises. "You can layer it in or use it for specific groups." Over time, that flexibility has proven effective. Data from the past five years show employees are often just as satisfied, or even more satisfied, with individual-market coverage. "There’s something to be said for that."
Expanding choices: ICHRA expands access to care, especially for employees spread across multiple states where traditional group plans often fall short. "Employees may find they don’t have any doctors in-network, or coverage may be limited far from the home base," Poole notes. "Once ICHRA is in place, employees have a much wider range of choices." For distributed workforces, that flexibility can translate directly into better access and fewer coverage gaps.
Making the market work: The effectiveness of ICHRA depends on administration with deep operational expertise. "Historically, there's been a stigma against the individual market, but the market is responding,” Poole shares. “Carriers are creating ICHRA-specific offerings that look more like group plans, with networks that cross multiple states.” These expanded networks and group-style structures help employers deliver a seamless experience while maintaining compliance and efficiency.
But even the best plan design can fail if employees don’t understand how to use it. Poole stresses that success requires a shift in how employers educate their teams. "Employers have an opportunity to communicate more about the benefits employees already have and how to use them," she notes, adding that awareness of the full range of benefits is currently often limited.
Benefits made simple: Poole emphasizes benefits literacy, education, and simpler plan designs. "Benefits plans are complex. To understand the math behind them, the devil is in the details. It’s not a fun topic, as nobody’s excited to calculate coinsurance," she acknowledges. When employees can grasp copays more easily than coinsurance or grasp common scenarios such as visiting a doctor, handling an accident, managing mental health, or welcoming a new child, they make smarter decisions. Thoughtful pairing with supplemental coverage strengthens both the benefits package and the employee experience.
Rollout with care: A measured rollout of new or redesigned benefits ensures smoother adoption and stronger engagement. Poole cautions against rushing the process. "Take time to plan your strategy, understand your employees’ knowledge and sophistication around health care and finances, and tailor your approach."
Guidance on demand: Employers can also provide expert support through patient advocates. "These are people with healthcare backgrounds whose entire job is to help employees navigate the complex healthcare system," Poole says. Partnering with these experts helps employees use their benefits effectively and reinforces the value of thoughtful plan design.
Emerging technology could simplify benefits even further, and Poole is optimistic about its potential. "There are growing forays into AI platforms for understanding benefits. Right now, I don’t think they’re quite there yet, but it’s rapidly changing." She encourages staying open-minded. "The industry is beginning to provide tools that help people understand their benefits in plain language," she concludes. "This is an opportunity for the market to create coordinated, holistic benefits so employees can clearly see how all the pieces work together."




.png)