All articles
With Group Plans Under Strain, ICHRA Offers Cost Certainty and Choice
As employer-sponsored group plans lose ground, Bruce Gilbert, CEO of BeWell New Mexico, explains the generational shift toward ICHRAs and what it signals for the future of benefits.
Key Points
The rising cost of traditional group health insurance is becoming unsustainable for many employers, forcing them to seek alternatives.
Bruce Gilbert, CEO of New Mexico's Health Insurance Marketplace, explains that this affordability crisis is driven by the "black box" of vertically integrated healthcare giants.
He details why a growing number of businesses are turning to ICHRAs to provide employees with tax-advantaged funds for their own plans, but notes how factors like political gridlock in Washington remain significant hurdles to widespread adoption.
The employer-sponsored health benefit world is absolutely in flux. Affordability is the biggest pressure point, and more employers are rethinking their whole benefits model.
The rising cost of traditional health insurance group plans is making the offering practically unsustainable for a large number of companies. In fact, 73% of employers in 2025 experienced more healthcare cost pressure than they had in over a decade, with many anticipating the highest health benefit cost in 15 years in 2026. The resulting pressure is forcing businesses to rethink their entire approach to providing coverage as they prepare.
Bruce Gilbert is an expert keeping track of this evolving healthcare ecosystem problem. As the Chief Executive Officer of BeWell, New Mexico's Health Insurance Marketplace, Gilbert oversees policy and direction for over 82,000 enrollees. An attorney with extensive experience in managing public health insurance exchanges, including his former role as Executive Director of Nevada's Silver State Health Insurance Exchange, he has a frontline view of the pressures forcing the market to change.
“The employer-sponsored health benefit world is absolutely in flux. Affordability is the biggest pressure point, and more employers are rethinking their whole benefits model," says Gilbert. According to him, the core of the problem driving this affordability challenge is a systemic "black box," where the vertical integration of a few massive healthcare players makes it difficult for employers and consumers to discern true costs and value.
An integrated empire: A small number of big companies controlling major parts of the healthcare system gives them enormous power over pricing, as Gilbert explains. "Look at UnitedHealthcare. They are not just a health insurer anymore. They have a pharmacy benefit manager in OptumRx and own provider groups and hospitals through Optum. You've seen this vertical integration with the largest players to the point where four or five of them now control health care in this country."
Cooking the books: He points out that regulations are supposed to limit how much insurers can profit, but vertical integration makes it unclear where costs are inflated. "The Affordable Care Act requires insurers to spend 85% of premium dollars on claims. But if you own the pharmacy, the physician practices, and the hospitals, you can make that happen really easily. That integration is driving a lot of the problems we're seeing."
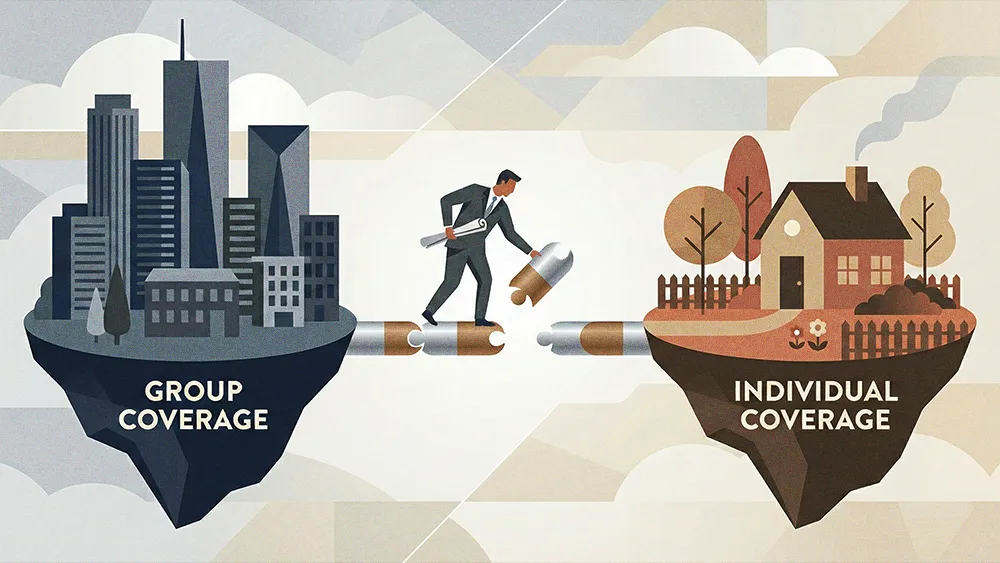
Financial pressure is mounting because many say the Affordable Care Act marketplace still isn’t meaningfully cutting costs in 2026. In response, a growing number of employers are turning to ICHRAs, seeing it as a way out of economic complexity. Since the model allows companies to provide tax-advantaged funds for employees to purchase their own coverage, it offers employers greater budget predictability and workers more choice.
The SHOP that flopped: "Most ACA marketplaces had a Small Business Health Options Program (SHOP) offering, but it hasn't been successful because it wasn't filling a need. The tax advantages were so small that people didn't see it as a viable option." Another key economic factor driving companies' embrace of ICHRA, Gilbert says, is that small group premiums grew roughly twice as fast as individual market premiums over the past five years. "The individual market has become more competitive, stable, and affordable, largely because of the ACA, and that's been a key driver behind the surge in ICHRA adoption."
Gilbert believes the rise of ICHRA reflects a deeper transformation in employer-sponsored benefits, one that could redefine how coverage is structured for years to come. But the runway to larger adoption is long-winding, thanks to the complexity of dizzyingly complicated systems being transferred to employees, outdated broker practices, and policy issues.
No one-click coverage: "People are used to an Amazon-like experience, but purchasing health insurance isn't simple," he says. "Providing that sort of an Amazon experience is essentially impossible. The best we can do is offer decision-making assistance and empower the end user to navigate that complexity." He likens the shift to when 401(k)s came to replace pension plans. Similar to that moment, it will potentially take three to five years before the ICHRA model becomes the norm.
Teaching old brokers new tricks: Another adoption hurdle is the traditional broker community. Gilbert notes for the model to scale, advisors must adapt. "There are very few brokers who know, understand, or are comfortable with an ICHRA-style product. For years, their model was offering large group or small group, so it's a completely different mindset." A future-forward broker, he says, will know how to position the offering according to employer needs, and highlight that "with this model, you decide how many dollars to spend, give that money to your employees, and you're out of the business of making those decisions."
Policy paralysis: Gilbert confirms that several state-based marketplaces, including his own in New Mexico, are actively exploring how they might integrate ICHRA-style platforms to better serve the small employer community. But he tempers market optimism with a dose of political reality, noting that legislative standstill creates operational uncertainty for insurers and employers. "I'm trying to understand what's going to come out of Washington in terms of coherent health policy because the truth is, no one knows where we're going. Everybody's waving their fist at each other and just yelling and screaming."
The result is an industry caught between clear market momentum and complete political paralysis, arriving at what many are seeing as an inflection point. "If we're not at a crossroads today, we are getting to a crossroads where the cost of providing coverage to folks through an employer is becoming prohibitively expensive," Gilbert concludes. "The question is, what happens next? And I don't think anybody knows."




.png)