All articles
Facing Volatile Renewals, Employers Turn To ICHRA As A Long-Term Cost-Control Strategy
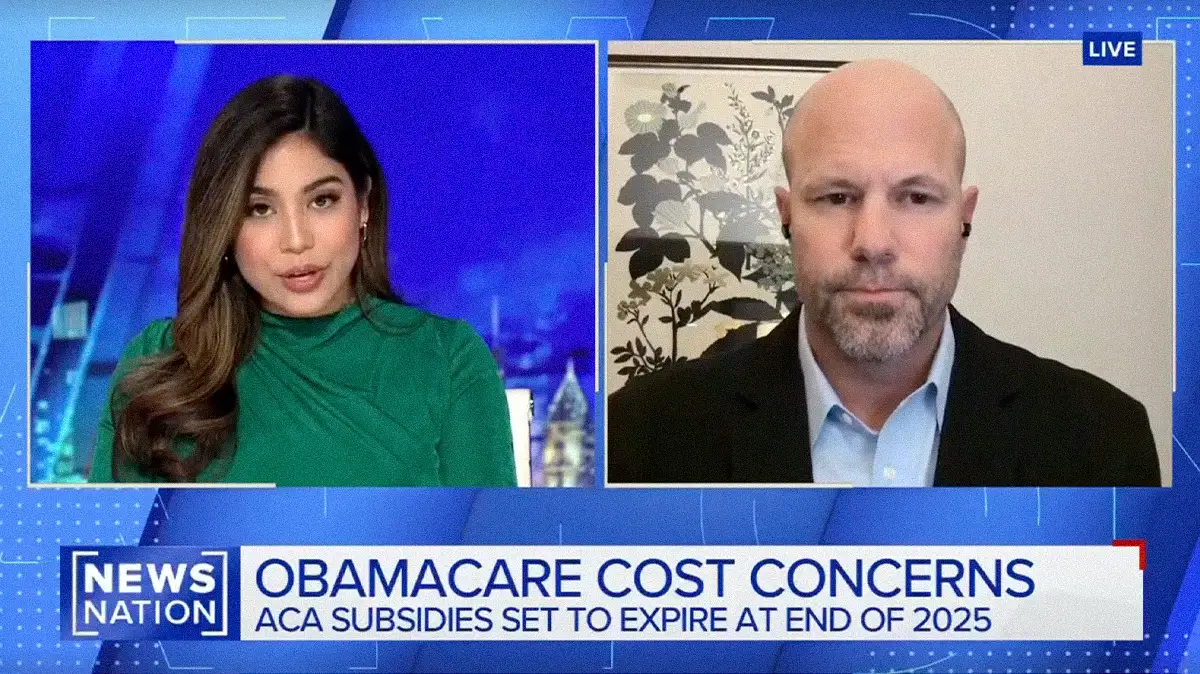
Michelle Mead, Head of Business Development at Leeway, explains why relentless healthcare cost inflation is pushing mid-sized employers to abandon "kick-the-can" renewal strategies in favor of budget-stabilizing models like ICHRA.

Key Points
Rising healthcare costs are pushing mid-sized employers past the breaking point, with annual premium increases of 20% to 60% making passive renewal strategies financially unsustainable.
Michelle Mead, Head of Business Development at Leeway, explains how ICHRA enables employers to set a defined benefits budget while shifting plan selection to employees, who can choose from dozens of individual market options.
The transition to ICHRA requires serious investment in employee education and change management, without which employers risk trading cost unpredictability for widespread confusion.
There is no cheap health insurance in the United States. It's one of the most expensive line items for every business, and ICHRA allows employers to normalize that cost while giving employees real ownership of their benefits.
For mid-sized employers, the familiar routine of absorbing another double-digit premium increase and revisiting strategy later is no longer viable. Healthcare is already one of the largest operating expenses on the books, and the compounding effect of successive 20%, 30%, even 50% annual increases is forcing a harder look at how benefits are structured.
Michelle Mead is the Head of Business Development at Leeway, a benefits administration platform focused on ICHRAs. A licensed insurance professional and HRA Council member, Mead has spent years working with employers navigating the transition from traditional group plans to defined contribution models.
"There is no cheap health insurance in the United States. It's one of the most expensive line items for every business, and ICHRA allows employers to normalize that cost while giving employees real ownership of their benefits," says Mead. The math, she says, is becoming impossible to ignore. An employee in their late 50s or early 60s can cost $1,400 per month for a mid-tier silver plan, while the same coverage for a younger employee runs closer to $450. For employers with aging workforces, traditional group plans concentrate that risk in ways that lead to volatile, sometimes catastrophic renewals.
The breaking point: Mead says the threshold is often predictable. "If an organization is paying over seven or eight hundred dollars a month per employee only on a composition program structure, ICHRA will almost always win." The kick-the-can approach might save 10% in a given year, but it adds risk with each renewal cycle. Mead has seen increases reach 50% to 60% for employers with high claims or older populations. "At some point, there's no more kicking the can. You're kind of like, 'All right, we've got to do something.'"
ICHRA flips the model. Instead of the employer selecting and funding a group plan, the employer sets a defined monthly contribution and employees purchase individual coverage. In Ohio, for example, employees can choose from roughly 127 different plan options. The employer's budget becomes predictable, and employees gain ownership over their plan selection.
The disconnect: But choice without comprehension creates its own problems. Mead notes a persistent literacy gap that undermines even well-designed benefit strategies. "They have no idea what that cost looks like. That's one of the things I think people are disconnected from, how much health insurance actually costs." Mead says the pattern is familiar: an employee pays $100 per paycheck and assumes that's the price, unaware that the plan runs $1,000 a month with the employer covering the difference. That disconnect breeds dissatisfaction regardless of how much the employer invests.
The solution, Mead argues, is pairing ICHRA with sustained education and change management. The shift from employer-selected plans to individual ownership requires employees to understand deductibles, out-of-pocket maximums, and how to match plan design to their actual health needs. Someone anticipating surgery might opt for a gold plan with lower cost-sharing. A younger, healthier employee might choose a bronze plan and pocket the difference.
Regulatory tailwinds: Momentum is building at the federal level. Mead expects ICHRA to be codified as a federal statute this year, potentially under a new name. "The acronym stands for Custom Health Options and Individual Care Expense. I've spent five years teaching people what ICHRA is and now we want to change it to Choice. But I like Choice a little bit better because it really does define it," says Mead.
For mid-sized employers caught between rising costs and limited leverage, the calculus is shifting. Passive renewal strategies that once bought time are now accelerating exposure. ICHRA offers a structural alternative, but only when paired with the education that makes employee ownership meaningful. "It really puts that power into the employee's hands," Mead concludes. "They can choose strategically based on what's happening in their health."





.png)